Ankylosing Spondylitis
Axial spondyloarthropathies including ankylosing spondylitis
What are ankylosing spondylitis and axial spondyloarthropathies?
These are generalized chronic inflammatory diseases, but their effects are seen mainly in the spine and sacroiliac joints. Definition have changed in the last decade to reflect the fact that ankylosing spondylitis (AS) is the end stage of a disease process best described by the term-axial spondyloarthropathy (axial SPA). AS is characterized by pain and stiffness of the back, with variable involvement of the hips and shoulders and (more rarely) the peripheral joints. Its reported prevalence is 0.1-0.2% in Western Europe and African peoples. Males are affected more frequently than females (estimates vary from 2:1 to 10:1) and the usual age is between 15 and 25 years.
Cause
There is considerable evidence regarding ankylosing spondylitis (AS) as a genetically determined immunopathological disorder. The disease is much more common in family members of patients who are suffering from the same or who have already suffered from it, than in the general population.
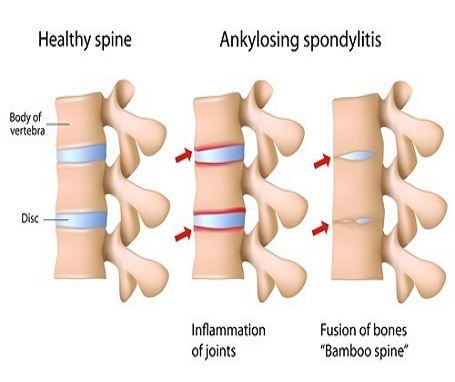
Pathology
There are two basic lesions: synovitis of diarthrodial joints and inflammation at the fibro-osseous junctions of syndesmotic joints and tendons. The preferential involvement of the insertion of tendons and ligaments (the entheses) has resulted in the term enthesopathy.
Synovitis of the sacroiliac and vertebral facet joints causes destruction of articular cartilage and periarticular bone. The costovertebral joints also are frequently involved, leading to diminished respiratory excursion. When peripheral joints are affected, the same changes occur.
Clinical Features
The disease starts insidiously: usually teenagers or young adults complain of backache and stiffness recurring at intervals over a number of years. This is often diagnosed as ‘simple mechanical back pain’ but the symptoms are worse early in the morning and after inactivity. Referred pain in the buttocks and thighs may appear as ‘sciatica’ and some patients mistakenly appear get treated for intervertebral disc prolapse. Gradually pain and stiffness become continuous and other symptoms begin to appear like-
- general fatigue
- pain and swelling of joints
- tenderness at the insertion of the Achilles tendon
- foot strain
- intercostal pain and tenderness.
Occasionally the disease starts with pain and slight swelling in a peripheral joint such as the ankle. Sooner or later, backache will come to the fore. In women, the axial skeletal disease may remain restricted to the sacroiliac joints making diagnosis challenging.
In the early stages, there is little to see apart from slight flattening of the lower back and limitation of extension in the lumbar spine. There may be diffuse tenderness over the spine and sacroiliac joints (occasionally) and tenderness of a single large joint.
- In established cases, the posture is typical: loss of the normal lumbar lordosis, increased thoracic kyphosis and a forward thrust of the neck; upright posture and balance are maintained by standing with the hips and knees slightly flexed, and in late cases these may become fixed deformities.
- Spinal movements are diminished in all directions, but loss of extension is always the earliest and the most severe disability. It is revealed dramatically by the ‘wall test’: the patient is asked to stand with his back to the wall; heels, buttocks, scapulae and occiput should all be able to touch the all simultaneously. If extension is seriously diminished, the patient will find this impossible.
- In the most advanced stage, the spine may be completely ankylosed from occiput to sacrum-sometimes in positions of grotesque deformity. Marked loss of cervical tension may restrict the line of vision to a few paces.
- Chest expansion, which should be at least 7 cm in young men, is often markedly decreased. In old people, who may have pulmonary disease, this test is unreliable.
- Peripheral joints (usually shoulders, hips and knees) are involved in over a third of the patients; they show the features of inflammatory arthritis-swelling, tenderness, effusion and loss of mobility. There may also be tenderness of the ligament and tendon insertions close to a large joint or under the heel.
- Extraskeletal manifestations, general fatigue and loss of weight are common. Acute anterior uveitis occurs in about 25% of patients. Other extraskeletal disorders, such as aortic valve disease, carditis and pulmonary fibrosis (apical), are rare and occur very late in the disease.
Treatment
The disease can be as damaging to a patient as rheumatoid arthritis but some continue to lead an active life. Treatment consists of-
(1) general measures to maintain satisfactory posture and preserve movement
(2) anti-inflammatory drugs to counteract pain and stiffness
(3) the use of TNF inhibitors for other cytokines such as IL-17 and IL-12/23 in development;
General measures:
Patient are encouraged to remain active and follow their normal pursuits. They should be taught how to maintain satisfactory posture. Apart from this, they must be urged to perform spinal extension exercises every day. Swimming, dancing and gymnastics are ideal forms of recreation. Rest and immobilization are contraindicated because they tend to increase the general feeling of stiffness.
TNF inhibitors:
With the introduction of the TNF inhibitors, it has become possible to treat the underlying inflammatory processes active in AS. This can result in significant improvement in disease activity including remission. These therapies are reserved for individuals who have failed to be controlled with non-steroidal anti-inflammatory drugs.