Osteoporosis
Uncovering osteoporosis
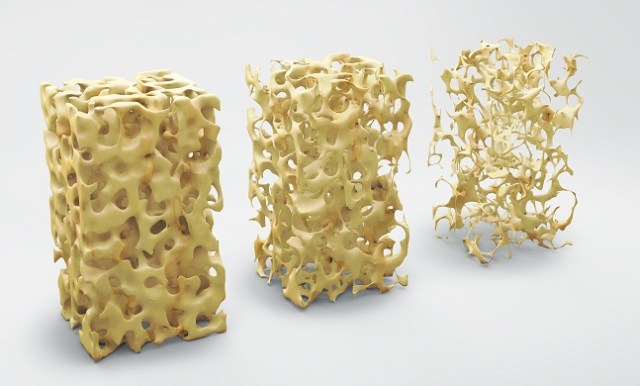
Due to higher incidences of fragility fractures and subsequent morbidity, osteoporosis has become a major public health problem. It is a condition that weakens bones, making them fragile and more likely to break. It develops slowly over several years and is often only diagnosed when a minor fall or sudden impact causes a bone fracture.
An estimated 1.3 million osteoporotic fractures occur in India every year. Though osteoporosis affects the entire skeleton, almost half of these fractures include hip and colles’ fractures. Hip Fractures occur as a result of minimal trauma or spontaneously (as in vertebral and occasionally hip fractures). They increase sharply in women after menopause and in men after 60 years of age.
Primary and secondary osteoporosis: Osteoporosis is defined by the medical literature as either primary or secondary.
- Primary osteoporosis: Primary osteoporosis is a bone disorder with an unknown origin which occurs at aging and accelerates at menopause. Approximately 95% of post-menopausal women and a majority of older men have primary osteoporosis. There is a threefold increase osteoclast activity (high turnover). Thus, an early menopause is a prominent promoter of osteoporosis. This results in an exponential increase in low trauma fractures. Advanced age is another important risk factor for the development of osteoporosis (senile osteoporosis). Senile osteoporosis is due to decreased osteoblast activity (low turnover). Additional risk factors for primary osteoporosis include-
– Caucasian race
- Age more than 50
- Family history of osteoporosis null parity
- Alcoholism
– Tobacco use
– Low physical activity
– Low calcium intake and vitamin D deficiency
- Secondary osteoporosis: Secondary osteoporosis has a direct cause. Glucocorticoids, with their extensive use, contribute to a large group of patients with secondary osteoporosis. Other factors include-
- Drugs (glucocorticoids, psychotropic drugs, anticonvulsant, heparin and oral anticoagulants, anti-retroviral drugs, aromatase inhibitors used in breast cancer and proton pump inhibitors)
- Endocrinopathies (hyperparathyroidism, hyperthyroidism, hypogonadism and insulin dependent diabete mellitus)
- Immobilization
- Liver cirrhosis
– Malabsorption syndromes
– Chronic inflammatory disorder (rheumatoid arthritis, ankylosing spondylitis, Crohn’s disease)
– Malignancies.
How is osteoporosis related to menopause?
POSTMENOPAUSAL Osteoporosis
Postmenopausal osteoporosis is an exaggerated form of the physiological bone depletion that normally accompanies ageing and loss of gonadal activity. Around the menopause, and for the next 10 years, bone loss normally accelerates to about 3% per year compared with 0.3% during the preceding two decades. This is due to increased bone resorption and the withdrawal of oestrogen. Genetic influences play an important part in determining when and how this process becomes exaggerated, but a number of other risk factors have been identified.
Clinical features and investigations
Osteoporosis is asymptomatic unless fractures occur. The fractures are classically low trauma defined as a fall from standing height or less. Fracture of the distal radius (Colle’s fracture) is usually the first fracture to occur, followed by vertebrae and hip unless treatment is initiated. Osteoporotic vertebral fractures are particularly difficult to diagnose as they may be clinically silent. Less than a third of vertebral fractures are diagnosed, and this is an important healthcare gap because older women with vertebral fractures are at one of the highest risks of future fracture. In severe cases, significant height loss (often exceeding 4cm) and thoracic kyphosis can occur due to multiple vertebral fractures. However, milder height loss and smaller kyphosis are most commonly due to degenerative changes.
What to do?: All women should be advised on lifestyle choices to maintain healthy bones. These include diets rich in calcium and vitamin D, weight bearing physical activity and to avoid smoking and excessive consumption of alcohol. If necessary, the recommended daily requirements should be met by taking calcium and vitamin D supplements; these measures have been shown to reduce the risk of low-energy fracture in elderly women. Hormones replacement therapy (HRT) and calcitonin are no longer recommended as treatments to reduce fracture risk. Other ways include:
- Bisphosphonates: Bisphosphonates taken orally are now regarded as the first-line medication for reduction of fracture risk in postmenopausal women, although intravenous formulations are also available.
- Parathyroid hormone: Preotact and Teriparatide are anabolic agent which, when given in intermittently low doses can stimulate bone formation to a greater and earlier extent than bone resorption.
Indications for Bone Mineral Density (BMD) diminution include-
- Women aged 65 years and older.
- Postmenopausal women under 65 years of age with risk factors for fracture (rheumatoid arthritis, long term glucocorticoids and other drugs, low body mass index, previous fracture, family history of fragility fracture).
- Men aged 70 years and older.
- Men under age 70 with clinical risk factors for fracture (e.g. hypogonadism).
- All adults with a fragility fracture*.
*Fragility or low trauma fracture is one that occurs after a fall from a height equal to that of the individual.
Prevention of Osteoporosis
Healthy bones equal a happy life. In order to live yours, a number of ways are available which can help you in building strong bones and prevent osteoporosis. These include-
- A calcium rich diet: A diet rich in calcium can make your bones rich in strength. Going by this, it is very important to have the necessary calcium intake in order to reach the peak of bone density. Good sources of calcium include: low fat dairy products such as ice cream, milk, yogurt; dark green leafy vegetables like broccoli and spinach; almonds, tofu etc. Apart from that, foods with added calcium like cereals, breads and orange juice are a great way to go.
- Vitamin D: An important characteristic of vitamin D is its property to absorb calcium from your diet. In case there is lack of vitamin D, your body won’t be able to absorb calcium from the foods you intake and as a result of this, it will start absorbing calcium from your bones making them weaker. Vitamin D deficiency can be cured either through direct exposure to sunlight or consuming foods rich in the source. Various foods rich in Vitamin D include: egg yolks, saltwater fish, and liver. Taking vitamin D supplements in case of extreme deficiency can also help.
- Exercise: An important way to make your bones strong is exercising. Indulging into weight training exercises can help increase your bone density to a large extent. Apart from that, resistance exercises also get the job done. For people who haven’t exercised a lot during their adulthood and are now dealing with osteoporosis should get recommendations on the type of exercises they can do, from their doctor.
- Quit smoking: In people who smoke, their body don’t absorb calcium at the pace it is supposed to. As a result of this, they have a higher chance of developing osteoporosis. In women particularly, smoking can result into an early menopause which in turn makes the development of osteoporosis even worse. So, it is recommended that in order to prevent osteoporosis, smoking should be prohibited.
- Limit alcohol intake: Heavy drinkers are most likely to develop osteoporosis as consuming alcohol in abundance is bad for your bones no matter what your age is.