Rickets
What is rickets and osteomalacia?
Rickets and osteomalacia are different terms for the same disease. Inadequate mineralization of bone in children is called rickets. However in adults, the condition is termed as osteomalacia. Osteoid, throughout the skeleton is incompletely calcified, and the bone is therefore ‘softened’ (osteomalacia). This leads to an increase in bone fragility and fracture risk. It usually occurs when there is insufficient intake of vitamin D through diet or when the body is unable to properly absorb the vitamin D intake of an individual. Vitamin D absorption is essential as it is responsible for absorbing calcium that is required to maintain strong and healthy bones. In children, the growth plate is also disrupted and hence leads to characteristic deformities (rickets).
Causes of rickets and osteomalacia
The causes of rickets and osteomalacia involve-
- Vitamin D deficiency: It can be caused due to inadequate intake of vitamin D through diet. Apart from this, insufficient exposure to sunlight can also be a major cause of vitamin D deficiency as exposure to sunlight helps in natural production of vitamin D in our skin.
- Celiac disease: If due to some reasons your intestinal lining is damaged, your body will be unable to absorb nutrients including vitamin D and calcium from your food leading to their deficiency eventually.
- Kidney and liver disorders: Kidney and liver are responsible for the synthesis of vitamin D in your body. Any damage to them can be a cause of worry as it will interfere with the metabolism of vitamin D.
- Drugs: Certain drugs that are used to treat seizures can cause severe deficiency of vitamin D in the body and hence, osteomalacia.
Symptoms of rickets and osteomalacia
Rickets and osteomalacia can be an end result of the following symptoms-
- Bone pain in hips, lower back, pelvis, legs, ribs
- Irregular heart rhythms
- Numbness of arms, legs and around the mouth
- Spasms in hands and feet
- Muscle weakness
- Fragile bones which fracture easily
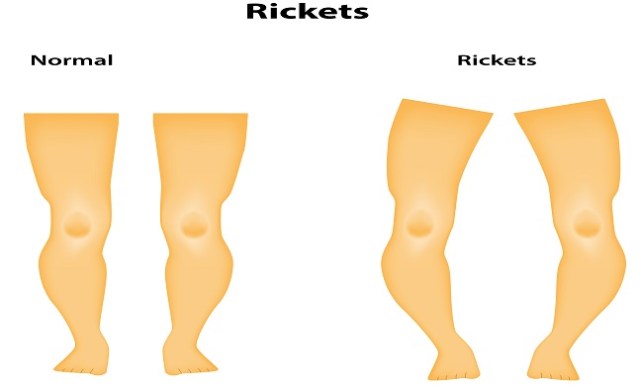
- Bow legs or knock knees
- Impaired growth
- Teeth defects including dental deformities and delayed tooth formation
- Delayed walking in children
- Increased cavities
- Poor muscle tone and development
Clinical features
Children: The infant with rickets may present with tetany or convulsions due to hypocalcaemia. Later the parents may notice that there is a failure to thrive, listlessness and muscular flaccidity. Early bone changes are deformity of the skull (craniotabes) and thickening of the knees, ankles and wrists from growth plate overgrowth. Enlargement of the costochondral junctions (rickety rosary’) and laetral indentation of the chest (harrison’s sulcus) may also be present. Lower limb deformities such as coxa vara and bowing of the femora and tibiae may develop after weight-bearing of the femora and tibiae may be stunted.
Adult: Osteomalacia may have an insidious course and patients may complain of relatively non-specific symptoms such as widespread bone pain and muscle weakness. Unexpected pain in the hip or one of the long bones may presage a stress fracture. Osteomalacia increases the risk of fractures throughout the skeleton. When present, muscle weakness. Osteomalacia increases the risk of fractures throughout the skeleton. When present, muscle weakness is of a proximal distribution, causing a ‘waddling’ gait.
X-rays
Children: In active rickets there is thickening and widening of the growth plate, cupping of the metaphysis and, sometimes, bowing of the diaphysis. The metaphysis may remain abnormally wide even after healing has occurred. If the serum calcium remains persistently low, there may be signs of secondary hyperparathyroidism: sub periosteal erosions are at the sites of maximal remodelling such as the redial aspects of the proximal and middle phalanges the middle and index fingers, medial borders of the proximal humerus, femoral neck, distal femur and proximal tibia.
Adults: The classical lesion of osteomalacia is the looser zone, a thin transverse band of rarefaction in an otherwise normal-looking bone. These zones, seen especially in the pubic rami, medial proximal femur and axillary edge of the scapula, are due to incomplete stress fractures which heal with callus-lacking in calcium. Vertebral fractures may show either a characteristic biconcave appearance or wedge-shaped deformities indistinguishable from osteoporotic fractures. There may also be signs of secondary hyperparathyroidism.
Treatment
In high-risk populations, osteomalacia is generally preventable by dietary modification or use of vitamin D supplements. For example, 400 IU per day is recommended in high-risk groups such as pregnant women. However, larger doses may be necessary in patients with malabrosption, in whom 25-OHD levels should be checked to confirm adequate replacement.
Prevention
The major prevention of osteomalacia involves adequate intake of vitamin D and calcium. Apart from this, sufficient exposure to sunlight also plays a key role.